3 Tricks for Your Nutrition if You’re Coming Off Antibiotics
Let’s start with the basics: What are antibiotics?
Antibiotics are a class of medicines used primarily to treat infections caused by bacteria in humans and animals. They can be classified into many different categories, but for the sake of simplicity, here are 2 ways to categorize your thoughts surrounding antibiotic types:
Broad-spectrum antibiotics: these target both harmful and non-harmful bacteria. These are associated with an increased risk for C-difficile or “C-diff” and a harsher side-effect profile.
Narrow-spectrum antibiotics: these are targeted antibiotics focused on killing specific bacteria and are recommended to be the first-choice prescribed by doctors since they do not target non-harmful bacteria and can therefore reduce the risk of antibiotic resistance and risk for infections (1-2).
Why would I need an antibiotic if I have Inflammatory Bowel Disease (IBD)?
Given that antibiotics are thought to play one of many possible roles in the development of IBD, and coupled with the historical over-prescribing of antibiotics and increased resistance to them, people are rightfully hesitant to take antibiotics (3-4). 2 things can co-exist: You can feel very valid discomfort surrounding the need for an antibiotic, and you can let your physician know if you feel this way. We should all be so lucky to be matched with a care team who takes our concerns into careful consideration. Here are some ideas to screenshot and bring to your care team if you have questions about being prescribed antibiotics:
If you have IBD, you might have been prescribed an antibiotic for some of these reasons:
Your body developed a bacterial infection
If you are awaiting a surgical procedure, including a cesarian section, antibiotics may be prescribed by your physician to reduce your risk for infection (5)
If you have inflammation in your gut related to primary sclerosing cholangitis (PSC), you may be on a longterm low-dose to help your body respond appropriately to the inflammation (6)
If you have a j-pouch with a history of pouchitis, antibiotics may have been prescribed to help. In this instance, antibiotics are not necessarily used to treat infection, so the primary indication for the antibiotic prescription changes. Instead, they’re prescribed to help the body respond to inflammation by decreasing the inflammatory load by altering the gut microbiome. (7)
Why so much hype around probiotics?
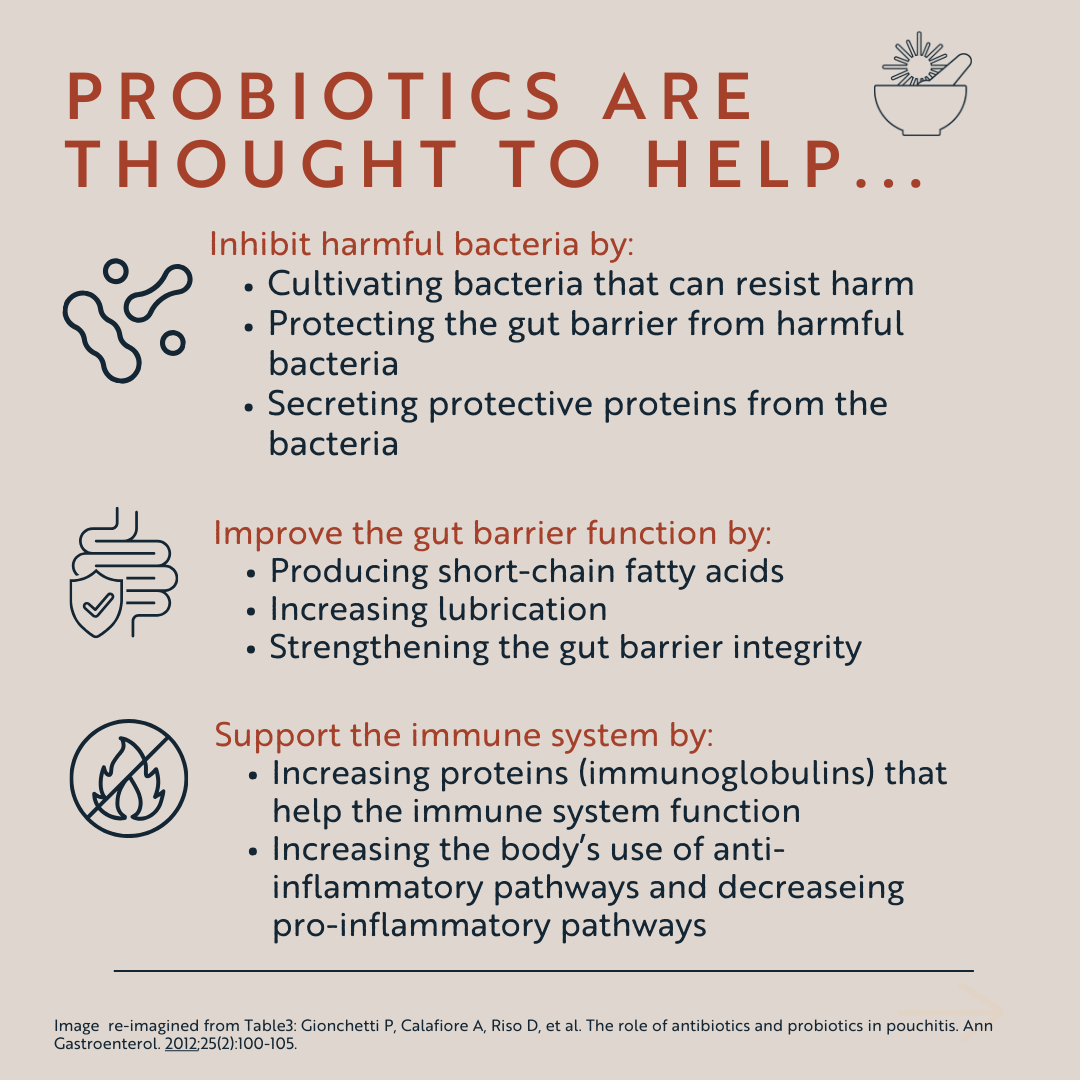
Microbiome bacterial diversity is SEXY, because it’s the closest definition that we have in research (right now) to defining a “healthy” microbiome. Probiotic foods can certainly help promote bacterial diversity and shift the microbiome toward health, and some supplements have been shown to do the same in certain instances. You can deep-dive to learn much more about probiotic foods, supplementation, and the microbiome in this post here. Below are some examples of how probiotics can help support the microbiome:
Do I need a probiotic supplement while on antibiotics?
Especially if you are on a broad-spectrum antibiotic, there is little to no benefit in beginning a probiotic while on an antibiotic, since the purpose of the antibiotic is to target all bacteria. There’s limited argument for the use of probiotics in this instance. You can read more about probiotics and how they function in this blog post.
Even if you are on a specifically targeted narrow-spectrum antibiotic, in my practice I do not tend to recommend adding in probiotic supplements, given that the research on the use of probiotics with antibiotics is not convincing to be beneficial at this time, and the potential cons out-weight the pros.
Here are 3 nutritional tricks to try as you come off antibiotics:
Even while on antibiotics, if you’re able to add probiotic-rich foods into your diet, now is the time!
Here’s why:For some, antibiotics can reduce the sensations associated with digestion, like gas and bloating, so antibiotics might make digesting foods and playing with gentle addition of foods a little easier, especially if you are someone who experiences digestive symptoms when adding in probiotic-rich foods.
You might not benefit much from the probiotic-specific effects while on antibiotics (that is, the recolonization of bacterial diversity), but if you’re able to expand your list of safe foods and add those to your rotation while on antibiotics, that’s going to serve you and your microbiome all the more when you come off antibiotics.
Unless directed by your doctor, do not take a probiotic supplement while on or coming off of antibiotics. Studies have shown that probiotics prolong the gut microbiome recovery period after antibiotics. Historically, probiotic supplementation while on antibiotics was thought to help manage unwanted antibiotic-associated symptoms, such as diarrhea, but more recent studies are showing that they are not helpful. (8, 9)
Food first! Most importantly, see this time coming off antibiotics as a time to support your microbiome by adding beautiful, colorful foods to your diet. Don’t skip the prebiotic foods, either (psst…there’s a whole post about prebiotic foods linked)! Prebiotics provide nutrition for the bacteria in your gut that are being added through your new-found probiotic safe foods. Below are some to consider adding during and after antibiotics, in addition to probiotic-rich foods.
To summarize:
Advocate for yourself by understanding why you need the antibiotic, for how long, and what to expect while taking the antibiotic. Discuss your hesitations (if any) with your GI care team.
Unless told otherwise by your medical doctor, do not take any probiotic supplements while on or coming off antibiotics. Instead, consider gently, intentionally adding probiotic (and prebiotic)-rich foods while on antibiotics so that they’re part of your safe foods when you’re off of the antibiotics.
Know that while, in theory, it’s a nice thought to support your microbiome through gentle addition of new foods, IBD makes this a valid challenge at times. If you feel like you could use support from a registered dietitian nutritionist, with understanding how to expand your diet safely and individualized to fit the needs of your body, feel free to reach out so we can work toward a solution for you. I have extensive experience living with IBD with limited support, helping people with IBD find safer ways to nourish their bodies, and I’ve received rigorous, formalized training in IBD nutrition. Here to help!
Frequently Asked Questions about Nutrition and Gut Health After Antibiotics
-
Antibiotics, especially broad-spectrum types, can disrupt the gut microbiome by eliminating both harmful and beneficial bacteria. This disruption may lead to decreased bacterial diversity, digestive discomfort, and an increased risk of infections like Clostridioides difficile.
-
The efficacy of probiotic supplements during antibiotic treatment is not well-established. Some research suggests that probiotics may help prevent antibiotic-associated diarrhea, but it's essential to consult with a healthcare provider before starting any supplement, as individual responses can vary.
-
Incorporating probiotic-rich foods can promote bacterial diversity and support gut health. Examples include:
Yogurt with live cultures
Kefir
Kimchi
Sauerkraut
Miso
These foods contain beneficial bacteria that may help restore balance to the gut microbiome.
-
After completing antibiotic treatment, gradually increasing fiber intake can support the growth of beneficial bacteria. Start with easily digestible sources like:
Oats
Bananas
Cooked vegetables
Over time, incorporate a variety of plant-based foods to promote microbial diversity and improve digestion.
-
Staying well-hydrated aids digestion and supports overall gut health. Water helps maintain the mucosal lining of the intestines and facilitates the movement of food through the digestive tract, promoting a balanced microbiome.
Implementing these nutritional strategies can help restore and maintain gut health following antibiotic treatment.
References:
Antimicrobial stewardship: systems and processes for effective antimicrobial medicine use. JAC Antimicrob Resist. 2019;1(2):dlz025. Published 2019 Jul 18. doi:10.1093/jacamr/dlz025
Antimicrobial stewardship: systems and processes for effective antimicrobial medicine use. JAC Antimicrob Resist. 2019;1(2):dlz025. Published 2019 Jul 18. doi:10.1093/jacamr/dlz025
Faye AS, Allin KH, Iversen AT, et al. Antibiotic use as a risk factor for inflammatory bowel disease across the ages: a population-based cohort study. Gut. 2023;72(4):663-670. doi:10.1136/gutjnl-2022-327845
Davis ME, Liu TL, Taylor YJ, et al. Exploring Patient Awareness and Perceptions of the Appropriate Use of Antibiotics: A Mixed-Methods Study. Antibiotics (Basel). 2017;6(4):23. Published 2017 Oct 31. doi:10.3390/antibiotics6040023
Williams MJ, Carvalho Ribeiro do Valle C, Gyte GM. Different classes of antibiotics given to women routinely for preventing infection at caesarean section. Cochrane Database Syst Rev. 2021;3(3):CD008726. Published 2021 Mar 4. doi:10.1002/14651858.CD008726.pub3
Du W, Han W, Dong J. Long-term oral vancomycin for refractory inflammatory bowel diseases without Clostridium difficile infection: Lessons from primary sclerosing cholangitis. Med Hypotheses. 2020;144:110211. doi:10.1016/j.mehy.2020.110211
Barnes EL, Agrawal M, Syal G, et al. AGA Clinical Practice Guideline on the Management of Pouchitis and Inflammatory Pouch Disorders. Gastroenterology. 2024;166(1):59-85. doi:10.1053/j.gastro.2023.10.015
Suez J, Zmora N, Zilberman-Schapira G, et al. Post-Antibiotic Gut Mucosal Microbiome Reconstitution Is Impaired by Probiotics and Improved by Autologous FMT. Cell. 2018;174(6):1406-1423.e16. doi:10.1016/j.cell.2018.08.047
Lukasik J, Dierikx T, Besseling-van der Vaart I, de Meij T, Szajewska H; Multispecies Probiotic in AAD Study Group. Multispecies Probiotic for the Prevention of Antibiotic-Associated Diarrhea in Children: A Randomized Clinical Trial [published correction appears in JAMA Pediatr. 2022 Jul 5;:null]. JAMA Pediatr. 2022;176(9):860-866. doi:10.1001/jamapediatrics.2022.1973