3 Reasons to Work with a Registered Dietitian Nutritionist BEFORE IBD Surgery
If you're preparing for surgey for IBD, such as Crohn's disease surgery, J pouch surgery, or ulcerative colitis surgery, you're probably feeling a mix of emotions—relief, anxiety, maybe even confusion about what comes next. That’s completely normal. One step you can take to support your recovery is working with a registered dietitian. Here’s why it matters:
Reason #1: Build Up Your Nutrition Before Surgery
Living with IBD (Crohn’s or colitis) can make it hard to get all the nutrients your body needs. Ongoing inflammation, poor appetite, or food restrictions may leave you undernourished going into surgery.
You deserve a whole-person nutritional approach before surgery even begins.
A dietitian can help you focus on the right foods to rebuild strength and address any nutrient gaps. Even small changes before surgery can support your immune system and help you heal more smoothly afterward.
This starts with a thorough assessment: Which risk factors do we need to address so that you have a better chance of recovering without complications? (1)
From a nutrition standpoint, we start by screening for malnutrition risk—ideally preventing it before it happens. Malnutrition is common in both Crohn’s disease and ulcerative colitis, even during remission, and it’s linked with poorer surgical and disease outcomes (2). The good news? A dietitian can help reduce those nutritional risks, setting you up for a smoother recovery. This is a basic level of care that anyone going into surgery deserves.
Here are a few other nutrition-related factors your dietitian will look out for:
Are you eating a complete diet with all essential nutrients?
Do you have any micronutrient deficiencies that need to be addressed before surgery?
Are you experiencing active inflammation that increases your nutrient needs—and is your current diet meeting those needs?
Do you need any texture modifications to stay safe before surgery (e.g. due to strictures)?
What does your lifestyle look like, and how can we build a practical plan to keep you nourished?
Are you the primary cook at home, and will that shift after surgery? Will caregiving responsibilities change?
What does your supplement routine look like, and can it be simplified?
How are you staying hydrated (e.g. water, tea, sports drinks)? How much and how often?
What type of surgery are you having, and how will it impact your ability to absorb nutrients?
Reason #2: Nutrition Can Support Your IBD Surgery Experience
Getting good nutrition before Crohn’s Disease surgery and other forms of IBD surgery, including j-pouch surgery doesn’t just help afterward—it can actually impact how your body handles the surgery itself. If you work with a dietitian to build a personalized supplement plan around your procedure, you may experience:
Lower risk of complications during or after surgery
More stable blood sugar levels during surgery
Faster return of stomach and intestinal function
Better overall healing
Fewer symptoms like nausea, vomiting, or bloating
A shorter hospital stay in some cases (3,4)
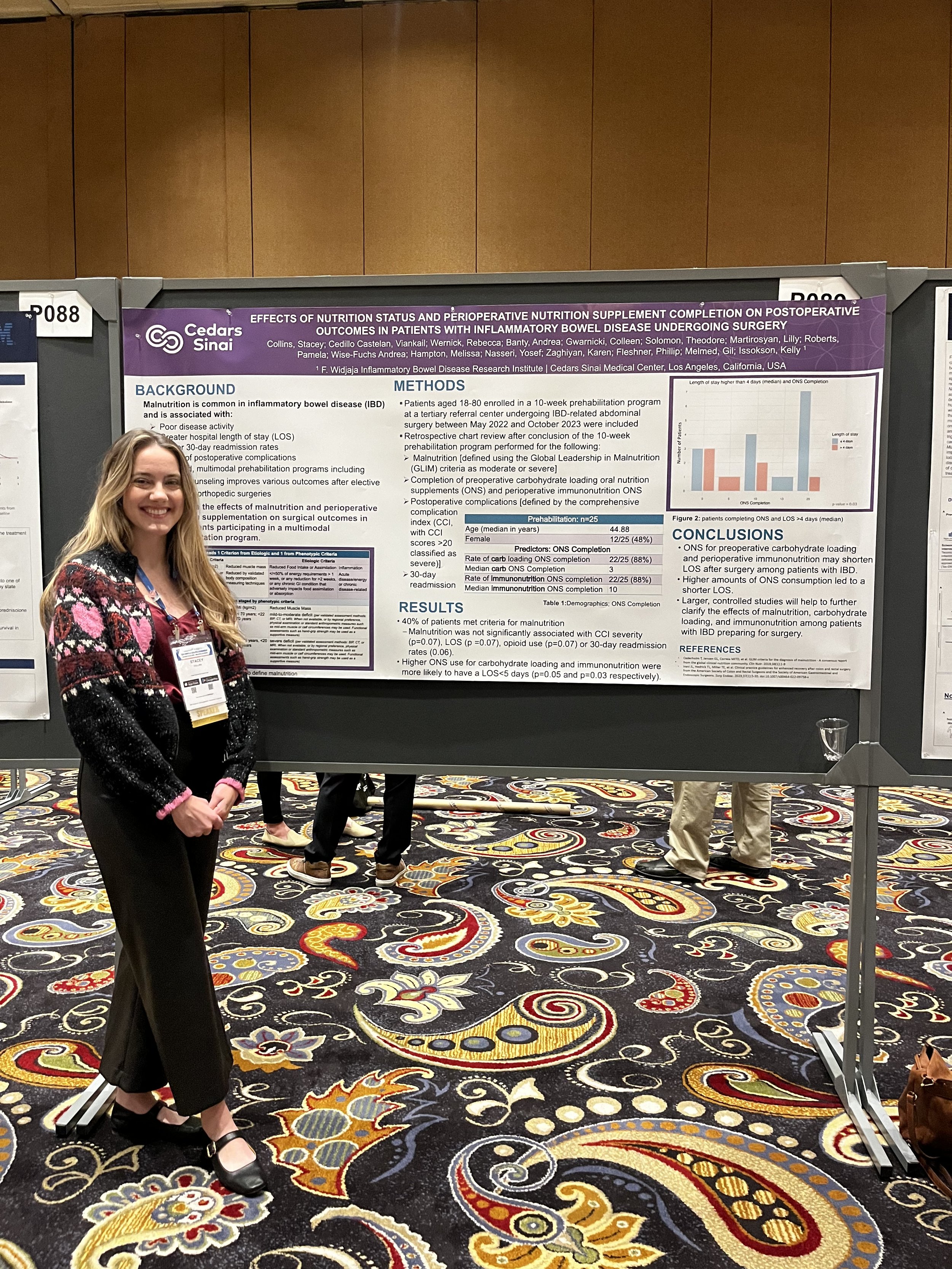
In fact, this is something I’ve collaborated on in research: Even patients who weren’t malnourished saw benefits. Those who were able to stick with the dietitian-guided supplement plan had shorter hospital stays after surgery (5).
Reason #3: Get Support to Stay Nourished and Strong After Surgery
Support from a registered dietitian nutritionist can help you get nourished and stay strong! Life awaits!
Surgery is meant to improve your quality of life—but sometimes the recovery process takes longer than it needs to. Why?
Because many people aren't just healing from surgery—they're also recovering from malnutrition.
It’s common to feel unsure about what or how much to eat after surgery. You might not know the best way to stay hydrated—yet proper hydration is one of the top reasons people end up back in the hospital after surgery (6).
You may also feel uncertain about how to eat safely: what textures are okay, how much is too much, and when to push forward or slow down. Too often, the guidance sounds like "eat whatever you want" or "just take it slow." And that’s not always helpful—especially if you've lived with a chronic GI condition and have a complicated relationship with food.
A dietitian understands this and can offer you specific, compassionate guidance so you can feel confident fueling your body as it heals.
If you’d like to be thoroughly assessed and properly supported before, during, and after surgery, please reach out to schedule a discovery call, where we can talk through your concerns and how I can help.
Not only do I have experience helping people through surgery: these are supports that I didn’t have and had to advocate for/give to myself while entering into/healing from 3-stages of J pouch surgery. Let me help you understand your body’s nutrition needs, what to anticipate, and how to navigate it all through individualized nutrition care.
References:
Carli F, Silver JK, Feldman LS, et al. Surgical Prehabilitation in Patients with Cancer: State-of-the-Science and Recommendations for Future Research from a Panel of Subject Matter Experts. Phys Med Rehabil Clin N Am. 2017;28(1):49-64. doi:10.1016/j.pmr.2016.09.002
Ünal NG, Oruç N, Tomey O, Ömer Özütemiz A. Malnutrition and sarcopenia are prevalent among inflammatory bowel disease patients with clinical remission. Eur J Gastroenterol Hepatol. 2021;33(11):1367-1375. doi:10.1097/MEG.0000000000002044
McAlee A, Allred J. Early Versus Traditional Oral Feeding Following Elective Colorectal Surgery: A Literature Review. Crit Care Nurs Q. 2021;44(2):147-159. doi:10.1097/CNQ.0000000000000349
Canzan F, Caliaro A, Cavada ML, Mezzalira E, Paiella S, Ambrosi E. The effect of early oral postoperative feeding on the recovery of intestinal motility after gastrointestinal surgery: Protocol for a systematic review and meta-analysis. PLoS One. 2022;17(8):e0273085. Published 2022 Aug 18.
Collins, Stacey et al. Effects of nutrition status and perioperative nutrition supplement completion on postoperative outcomes in patients with inflammatory bowel disease undergoing surgery. Poster presented at Crohn’s & Colitis Congress; Jan 25-27, 2024; Las Vegas
Chen SY, Stem M, Cerullo M, et al. Predicting the Risk of Readmission From Dehydration After Ileostomy Formation: The Dehydration Readmission After Ileostomy Prediction Score. Dis Colon Rectum. 2018;61(12):1410-1417. doi:10.1097/DCR.0000000000001217