How Nutrition Can Help with Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) is a chronic condition that affects the gastrointestinal (GI) tract, leading to inflammation, discomfort, and disruptions in daily life. Many people mistakenly use the term irritable bowel disease, but this is not a medically recognized condition. Instead, IBD includes Crohn’s disease, ulcerative colitis, microscopic colitis, and indeterminate colitis—each with unique challenges and treatment approaches.
When it comes to managing IBD, nutrition plays a crucial role in symptom relief, aiding in anti-inflammation, supporting gut health, and improving overall well-being. While diet alone may not induce remission, it can complement medical treatments and help maintain a balanced gut environment.
Let’s dive into how nutrition can support IBD management and explore foods that may either worsen gut inflammation or help reduce it.
Let’s Start with the Basics: What Is Inflammatory Bowel Disease (IBD)?
IBD, or Inflammatory Bowel Disease, is a group of chronic conditions that cause inflammation in the intestines. The two main types are Crohn’s disease (CD) and ulcerative colitis (UC). Some people receive a diagnosis of indeterminate colitis when their symptoms don’t clearly fit into either category.
Other forms of IBD include microscopic colitis (MC) and Intestinal Behcet’s disease (BD), though there is debate about whether Behcet’s disease meets the strict definition of IBD.
A key characteristic of IBD is ongoing cycles of inflammation in the gastrointestinal (GI) tract, leading to periods of flare-ups (active disease) and remission (no disease activity). Because symptoms can range from mild to severe—and don’t always match the level of inflammation present—regular monitoring is essential to prevent disease progression.
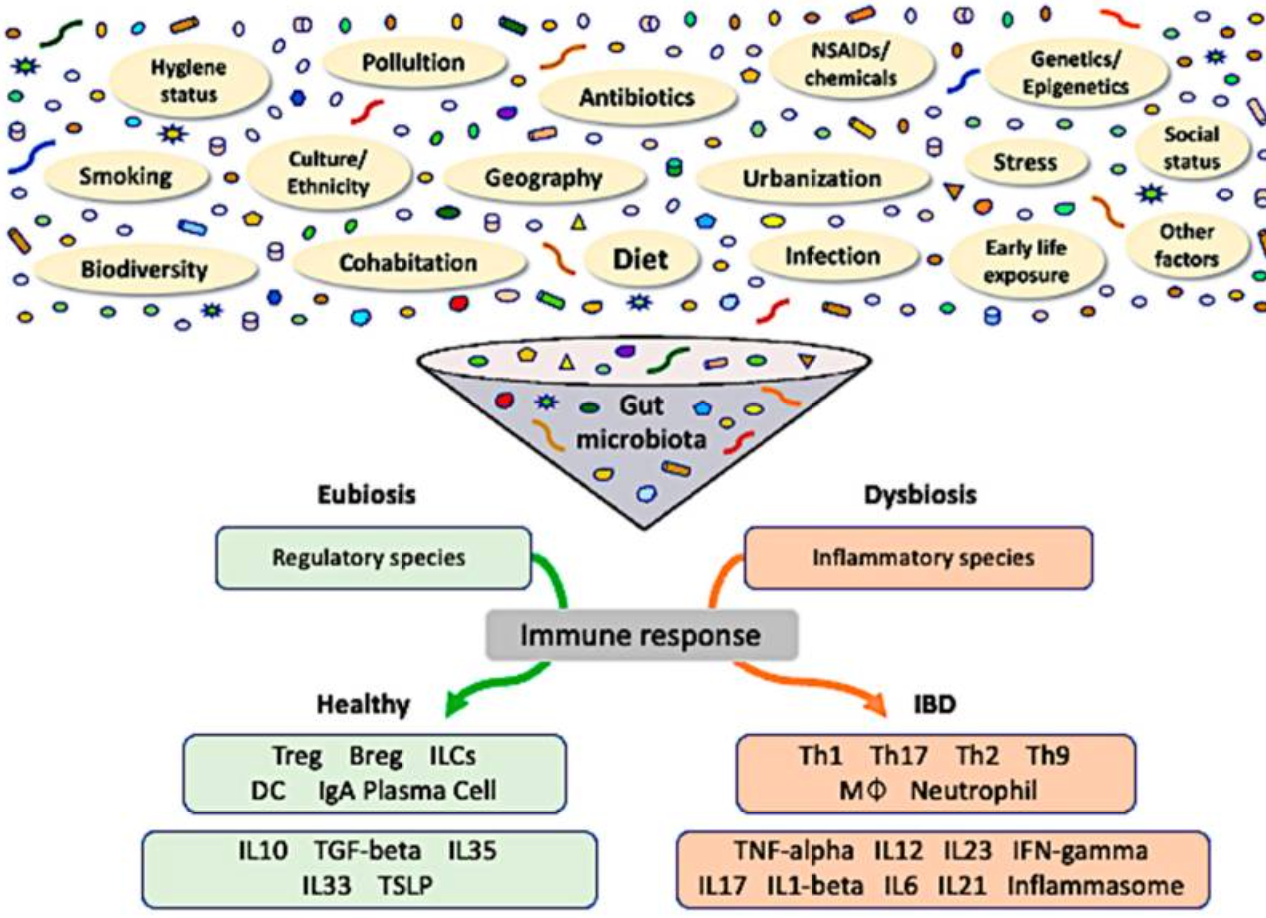
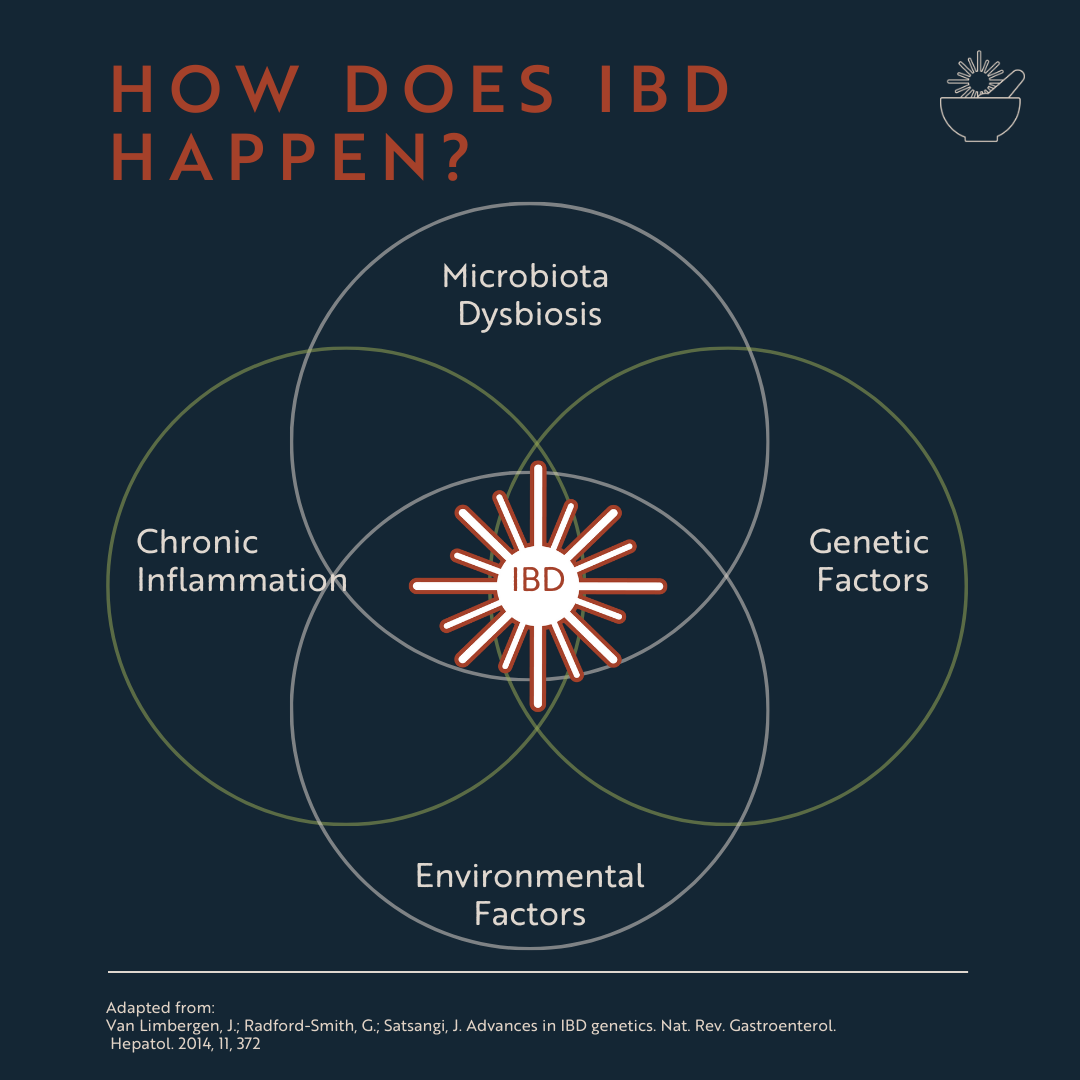
How Does IBD Happen?
In people who are genetically predisposed, IBD develops due to an abnormal immune response to gut microflora—the bacteria, fungi, and microbes that make up the gut microbiome.
A lack of bacterial diversity in the gut can lead to dysbiosis, where harmful bacteria outnumber beneficial ones. This imbalance, combined with genetic susceptibility, can be triggered or worsened by factors such as:
Psychological stress
Diet and eating patterns
Smoking
Gastrointestinal infections
Certain medications
Urban living environments
Geography
Social and economic factors
Ethnicity
This gut imbalance triggers an immune response, leading to inflammation and symptoms that can vary from person to person. Common symptoms of IBD include:
✔️ Diarrhea
✔️ Constipation
✔️ Abdominal pain and cramping
✔️ Blood or mucus in the stool
✔️ Nausea and vomiting
✔️ Unintentional weight loss
✔️ Delayed growth in children
✔️ Fatigue
✔️ In some cases: bowel obstructions, strictures, fistulas, or abscesses
How Is IBD Diagnosed?
Since symptoms alone don’t always indicate IBD, a formal diagnosis requires medical testing. The gold standard is an endoscopy or colonoscopy, performed by a gastroenterologist (GI doctor), colorectal surgeon, or, in some cases, an internal medicine specialist.
In short, IBD results from a combination of genetics, environmental factors, and gut bacteria imbalances—and early diagnosis and management are key to preventing complications.
How Can Nutrition Help with IBD Symptoms?
Nutrition plays a key role in managing symptoms of IBD, improving energy levels, and supporting overall well-being. Here are three ways nutrition can make a difference:
1. How Nutrition Can Help Reduce Fatigue
Up to 80% of people with IBD experience severe fatigue, which can make daily tasks feel exhausting. A well-balanced diet, combined with micronutrient monitoring, can help manage energy levels.
During a nutrition assessment, a dietitian can identify potential micronutrient deficiencies linked to fatigue and work with your GI care team to address them. Based on lab results, they may recommend:
Specific supplements (iron, vitamin B12, vitamin D, are important to monitor)
Best intake method (oral supplements, IV therapy, or dietary changes)
Proper dosage and duration to correct deficiencies
Other Ways to Manage Fatigue in the Kitchen
When energy levels are low, cooking can feel overwhelming. Here are easy meal prep strategies to help:
Cooking Hacks
One-Pot & Sheet Pan Meals – Minimal prep, minimal cleanup. Just toss everything in!
Slow Cooker or Instant Pot – Dump-and-go recipes save time and effort.
Frozen Ingredients – Pre-chopped veggies, cooked grains, and proteins (like rotisserie chicken or frozen meatballs) can be lifesavers.
Pre-made Sauces & Marinades – Adds flavor without extra effort.
Double Up – Cook larger portions when you have energy and freeze extras for later.
Prepping Hacks
Buy Pre-chopped or Pre-washed Produce – A little pricier, but saves tons of effort.
Use Kitchen Gadgets – Food processors, garlic presses, and peelers reduce manual work.
Batch Prep on Good Days – Chop veggies, cook proteins, and portion out snacks when you’re feeling up to it. Ask for help from family or friends, and put on a good playlist!
Assemble, Don’t Cook – Try Bento boxes, wraps, or sandwiches that require little to no cooking.
Consider Meal Kits – If budget allows, pre-portioned meal kits make cooking easier.
2. How Nutrition Can Help with Diarrhea and Constipation
Have you ever been told to avoid fiber because of IBD? You’re not alone!
For years, people with IBD were advised to follow low-fiber or low-residue diets, but this advice often led to missing out on anti-inflammatory foods that could actually help manage symptoms.
The truth? Fiber is complex, and different types, textures, and amounts can impact IBD symptoms in different ways. Instead of avoiding fiber altogether, it’s about finding the right fiber modifications that work for your body.
3. How Nutrition Can Help with Nausea
Nausea and vomiting are common in Crohn’s disease and can also occur in ulcerative colitis, especially due to inflammation or medication side effects. While nausea can make eating difficult, the right nutrition strategies can help ease symptoms and maintain adequate nutrition.
Tips for Managing Nausea
Adjust Your Eating & Drinking Habits
Space out liquids — Avoid drinking with meals. Instead, wait 30–60 minutes before or after eating to prevent bloating and nausea.
Stay upright after meals — Lying down immediately after eating can trigger acid reflux and worsen nausea.
Chew slowly and thoroughly — This helps digestion and reduces strain on your intestines.
Ask for help with cooking — Preparing food when nauseated can be overwhelming. If possible, let a friend or family member assist.
Foods to Avoid When Nauseated
Certain foods can worsen nausea by irritating the stomach or being harder to digest:
❌ Greasy, fried foods – Heavy and difficult to break down.
❌ Acidic or spicy foods – Citrus fruits, tomatoes, and spicy dishes may aggravate nausea.
❌ High-fat foods – Cream-based pasta sauces, beef, and pork can be harder to digest.
Foods That Help With Nausea
Anti-Nausea Herbs & Spices
✔️ Ginger — Well-studied for its anti-nausea effects; try ginger tea, chews, or fresh ginger in meals.
✔️ Mint & fennel — Can help soothe the stomach and reduce nausea.
✔️ Rosemary, thyme, parsley, and cinnamon — Gentle on digestion and may ease nausea.
Small, Frequent Meals
Eating small meals throughout the day rather than large portions can ease digestion and prevent nausea from worsening. Skipping meals can make nausea worse, so try to eat even if your appetite is low.
Electrolyte-Rich Foods
Nausea and vomiting can lead to electrolyte imbalances. Replenish key nutrients like potassium and magnesium:
✔️ Potassium-rich foods — Bananas, potatoes, melons, tomatoes (once nausea subsides).
✔️ Magnesium-rich foods — Nut butter, hummus, whole grains (breads, pastas, crackers).
Managing Nausea During Pregnancy with IBD
If you’re pregnant and dealing with IBD-related nausea, talk to your doctor about Vitamin B6 or ginger supplements—both can be effective in reducing nausea. However, do not take supplements without consulting your healthcare provider, as some may have unintended side effects.
Key Insights for Managing IBD with Nutrition
IBD is a complex disease influenced by genetics, environment, and gut health.
Regular monitoring is crucial, even during remission, as symptoms don’t always reflect disease activity.
Nutrition plays a powerful role in symptom management, helping with:
Fatigue relief
Managing diarrhea and constipation (Yes, fiber is important!)
Easing nausea with strategic food choices
Can nutrition impact inflammation? Yes! Diet can play a role in both inducing and maintaining remission, which will be explored in an upcoming post.
By personalizing your diet, you can reduce symptoms, support gut health, and improve your quality of life with IBD.
Frequently Asked Questions on Nutrition for IBD
-
IBD (Inflammatory Bowel Disease) are chronic inflammatory diseases of the digestive tract that includes Crohn’s disease, ulcerative colitis, and microscopic colitis. IBD can lead to intestinal damage and complications.
IBS (Irritable Bowel Syndrome) is a functional gut disorder that affects bowel movements but does not cause damage to the intestines in the way that IBD can.
-
Trigger foods vary by person, and it is important to note that symptom triggers do not always correlate with the worsening of inflammation. For example, garlic, onion, and coffee all promote anti-inflammatory benefits, however, garlic and onion might make gas worse/more sensitive during active disease flares. Coffee is liver protective and anti-inflammatory, although it can act as a stimulant laxative and therefore can give the illusion that the disease is more inflammatory, when in reality it is exacerbating symptoms, but not the disease itself.
Eating patterns matter more than individual ingredients! Focus on limiting exposure to foods that may correlate with worsening of disease activity:
❌ Ultra-processed foods (packaged snacks, fast food, and additives, like carboxymethylcellulose, polysorbate80, maltodextrin, and carageenan)
❌ Fried and greasy foods
❌ Sugar-sweetened beverages
❌ Red and processed meats
❌ Artificial sweeteners (like sorbitol and sucralose)
-
Diet can help manage symptoms and support remission, but for most people, it cannot replace medical treatment. A combination of diet, medication, and lifestyle modifications is usually needed for long-term disease management.
-
Certain foods may help calm inflammation and support gut health, including:
Omega-3-rich foods – Salmon, flaxseeds, walnuts (walnut butter), chia seeds
Probiotic foods – Yogurt, kefir, fermented vegetables
Vegetables (cooked veggies are great if tolerated better in a flare, fork-tender against the roof of your mouth) – Carrots, zucchini, squash
Resistant starch- greener bananas (if tolerated), cooked and cooled potato, oats, and rice
Fruits- Berries (mashed if better tolerated), Bananas, (peeled if in an active flare) apples, melons
-
Fatigue is common in IBD and can be linked to micronutrient deficiencies like iron, vitamin D, and B9 and B12. Work with a dietitian to:
Identify nutrient deficiencies
Adjust your diet or supplements accordingly
Use energy-saving meal prep strategies (one-pot meals, batch cooking, pre-chopped ingredients)
-
If nausea is an issue, try:
Eating small, frequent meals
Avoiding greasy, spicy, and acidic foods
Incorporating nausea-fighting herbs like ginger, mint, and fennel
Replenishing electrolytes with bananas, potatoes, and nut butter
-
Yes! Chronic diarrhea, vomiting, and inflammation can lead to dehydration and electrolyte imbalances. Drink 8–10 glasses of water per day and include 8×16 oz of electrolyte-rich beverages, salting foods to maintain hydration if you are running to the bathroom with urgent, liquid bowel movements more often than not.
-
Yes! An IBD-experienced dietitian can help tailor your diet to:
✔️ Reduce symptoms (diarrhea, constipation, nausea, fatigue)
✔️ Support medication effectiveness
✔️ Prevent malnutrition and deficiencies
✔️ Promote a better relationship with food
✔️ Ensure a balanced diet during flares and remission
CITATIONS
McDowell C, Farooq U, Haseeb M. Inflammatory Bowel Disease. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470312/
Santana PT, Rosas SLB, Ribeiro BE, Marinho Y, de Souza HSP. Dysbiosis in Inflammatory Bowel Disease: Pathogenic Role and Potential Therapeutic Targets. Int J Mol Sci. 2022;23(7):3464. Published 2022 Mar 23. doi:10.3390/ijms23073464
Kim DH, Cheon JH. Intestinal Behçet's Disease: A True Inflammatory Bowel Disease or Merely an Intestinal Complication of Systemic Vasculitis?. Yonsei Med J. 2016;57(1):22-32. doi:10.3349/ymj.2016.57.1.22
Dahal RH, Kim S, Kim YK, Kim ES, Kim J. Insight into gut dysbiosis of patients with inflammatory bowel disease and ischemic colitis. Front Microbiol. 2023;14:1174832. Published 2023 May 11. doi:10.3389/fmicb.2023.1174832
Uhlir V, Stallmach A, Grunert PC. Fatigue in patients with inflammatory bowel disease-strongly influenced by depression and not identifiable through laboratory testing: a cross-sectional survey study. BMC Gastroenterol. 2023;23(1):288. Published 2023 Aug 22. doi:10.1186/s12876-023-02906-0
Massironi S, Viganò C, Palermo A, et al. Inflammation and malnutrition in inflammatory bowel disease. Lancet Gastroenterol Hepatol. 2023;8(6):579-590. doi:10.1016/S2468-1253(23)00011-0
Gkikas K, Gerasimidis K, Milling S, Ijaz UZ, Hansen R, Russell RK. Dietary Strategies for Maintenance of Clinical Remission in Inflammatory Bowel Diseases: Are We There Yet?. Nutrients. 2020;12(7):2018. Published 2020 Jul 7. doi:10.3390/nu12072018
Haskey N, Gold SL, Faith JJ, Raman M. To Fiber or Not to Fiber: The Swinging Pendulum of Fiber Supplementation in Patients with Inflammatory Bowel Disease. Nutrients. 2023;15(5):1080. Published 2023 Feb 21. doi:10.3390/nu15051080
Godny L, Maharshak N, Reshef L, et al. Fruit Consumption is Associated with Alterations in Microbial Composition and Lower Rates of Pouchitis. J Crohns Colitis. 2019;13(10):1265-1272. doi:10.1093/ecco-jcc/jjz053
He L, Fan Y, Hu Y, et al. The potential hazards of high doses of vitamin B6 in treating nausea and vomiting in pregnancy: A systematic review. Int J Gynaecol Obstet. Published online November 21, 2024. doi:10.1002/ijgo.16032
Viljoen E, Visser J, Koen N, Musekiwa A. A systematic review and meta-analysis of the effect and safety of ginger in the treatment of pregnancy-associated nausea and vomiting. Nutr J. 2014; 13:20.
Haniadka R, Popouri S, Palatty PL, Arora R, Baliga MS. Medicinal Plants as Antiemetics in the Treatment of Cancer: A Review. Integrative Cancer Therapies. 2012;11(1):18-28. doi:10.1177/1534735411413266